Features
Topics
Discover
Unlock the potential of your career in the Pharma industry with our online courses and qualifications.

Career Path
Pick a career path, follow its guided course roadmap, and secure industry-verified credentials in a few months.

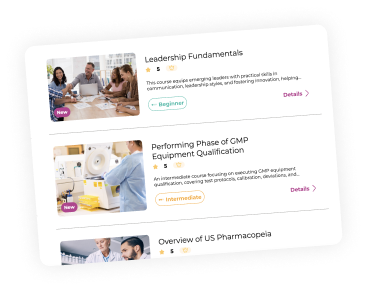
Courses
Earn career credentials from industry leaders that demonstrate your expertise.