Digital marketing in pharma and medtech is no longer optional. It’s a necessity. As patients, healthcare professionals, and regulators move online, companies must adapt their strategies. Traditional methods such as printed brochures or conference-only engagement don’t deliver the same reach or impact anymore. Today’s audiences expect personalized, compliant, and on-demand information.
The digital transformation in healthcare marketing is speeding up. Pharma and medtech companies are investing in digital channels to improve reach, streamline communication, and stay compliant with evolving global regulations. Additionally, digital tools help marketers gain real-time insights about what works and what doesn’t.
This shift has created new opportunities but also introduced new rules. Unlike fashion or retail marketing, healthcare marketing must follow strict regulations. Every tweet, banner ad, or landing page must align with compliance guidelines. That’s where smart digital marketing strategies come in—helping teams stay innovative and compliant at the same time.

What’s Driving Digital Marketing in Pharma & MedTech?
The need to deliver accurate, engaging, and compliant information drives digital marketing in pharma and medtech. Regulation changes, patient empowerment, and digital maturity all shape the strategies that marketers now use.
In the past, sales reps were the main point of contact for doctors. Today, HCPs (healthcare professionals) prefer digital interactions. They visit company websites, read white papers, and watch short videos when it suits them. That means pharma companies must be ready with multichannel content tailored to different user needs.
Meanwhile, patients want more control over their health journeys. They use search engines, online forums, and YouTube to learn about treatment options. Medtech marketers must now develop direct-to-patient content while staying compliant with advertising laws.
Compliance plays a big role too. Regulators like the FDA and EMA require companies to document digital activities. Marketers must show they’re not making false claims or hiding risks. So, digital marketing in pharma and medtech must blend creativity, science, and regulatory knowledge in every campaign.
Top Trends in Digital Marketing for Pharma & MedTech
Here are the leading trends shaping digital marketing in pharma and medtech today:
- Omnichannel Campaigns - Marketers now use multiple platforms—email, webinars, social media, and apps—to create consistent experiences across channels.
- Personalized Content - AI tools help tailor messages to HCPs and patients based on behavior, specialty, or diagnosis.
- Video-Based Learning - Short videos and animations are replacing PDFs. Videos improve retention and simplify complex topics.
- SEO-Driven Content - Companies now invest in keyword-optimized blogs and glossaries to appear in search results organically.
- Virtual Events & Webinars - Webinars offer live interaction and education without the cost of physical conferences.
- Mobile-First Strategies - With most users accessing content via smartphones, pharma marketers are designing mobile-optimized landing pages and apps.
- Social Listening - Teams monitor platforms like LinkedIn and Reddit to understand audience sentiment and trends.
- CRM & Automation - Automated email journeys based on CRM data allow better segmentation and engagement tracking.
- Regulatory-Ready Digital Assets - Templates and checklists ensure every marketing asset can pass internal and external review.
- Data Analytics and ROI Tracking - Real-time dashboards help teams track performance, A/B test content, and make data-driven decisions.
A Closer Look at Omnichannel and Personalization
Omnichannel and personalization are no longer just marketing buzzwords—they are essential strategies for pharma and medtech brands. In regulated industries, trust and timing matter. These two approaches ensure that you reach the right person, in the right way, at the right time. That’s why companies that apply both strategies outperform those relying on outdated one-size-fits-all campaigns.
Today’s healthcare professionals and patients interact with brands across multiple platforms. From mobile apps to webinars, they expect consistent messaging and personalized experiences. To meet this demand, marketers must build journeys that feel seamless and relevant. Omnichannel ensures consistency; personalization brings relevance. Together, they elevate engagement, increase conversion rates, and strengthen brand loyalty.
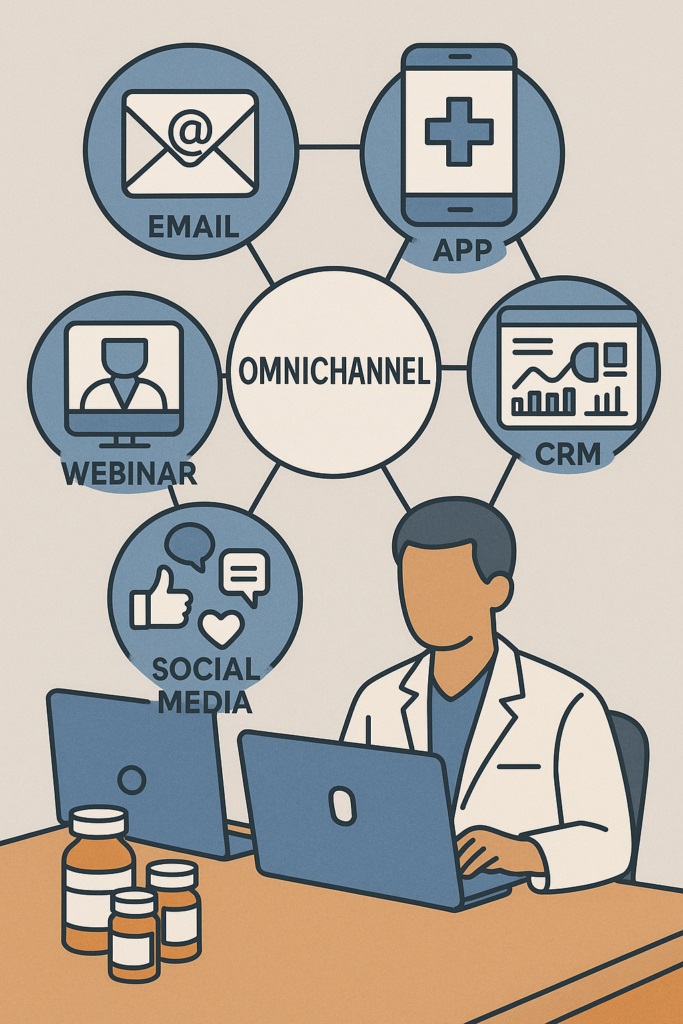
Omnichannel Engagement: Delivering a Consistent Experience Everywhere
Omnichannel marketing creates a unified customer journey across platforms. It connects your channels into one seamless story.
- Email + Web + Social: Coordinate messages across email campaigns, landing pages, and social media.
- HCP Portals: Offer consistent, gated content with personalized logins for healthcare professionals.
- Live & On-Demand Events: Run webinars that link back to whitepapers and post-event surveys.
- Sales & CRM Integration: Equip field reps with insights from digital touchpoints to tailor follow-ups.
- Regulatory Review: Apply standard templates to ensure every asset is compliant across channels.
Omnichannel strategy reduces confusion, improves user satisfaction, and supports more efficient internal workflows.
Personalized Content: Relevance That Converts
Personalization means showing the right message to the right audience based on real needs and behaviors.
- HCP Segmentation: Target based on specialty, location, or prescribing behavior.
- Patient Profiles: Adapt content for demographics, disease state, or treatment stage.
- Behavior Triggers: Send follow-ups when users click, download, or attend a webinar.
- Dynamic Email Content: Customize sections within emails based on recipient data.
- Preferred Channels: Respect user preferences—email for some, mobile notifications for others.
Personalized marketing builds trust, increases relevance, and boosts click-through and conversion rates consistently.

Key Tools That Power Digital Marketing in Pharma & MedTech
Here are essential tools helping marketers scale smartly:
- Marketing Automation Platforms (MAPs) - Automate email workflows, landing pages, and engagement.
- Customer Relationship Management (CRM) Systems - Track HCP or patient data and interactions
- Compliance Review Platforms - Tools can streamline the review of materials by legal, medical, and regulatory teams.
- SEO and Analytics Software - Platforms like SEMrush, Ahrefs, and Google Analytics guide content strategies and performance reviews.
- Survey and Feedback Tools - Collect real-time feedback from users using Typeform or Qualtrics to guide content development.
- Content Management Systems (CMS) - WordPress and Drupal allow scalable content publishing across global teams with approval flows.
- Webinar Hosting Tools - Zoom Webinars or ON24 support compliant, interactive sessions with healthcare audiences.
- Social Media Monitoring Tools - Use this tools to monitor discussions, measure sentiment, and engage professionally.
- eLearning Platforms - Platforms like Pharmuni offer structured learning for marketers and medical teams.
- Chatbots and Conversational AI - Use AI assistants to guide users, answer product questions, or provide onboarding support 24/7.
The Rise of Digital Ethics and Innovation
As digital tools become more powerful, pharma and medtech marketers must balance innovation with responsibility. Every new channel, algorithm, or campaign introduces ethical decisions. Missteps can erode trust or lead to regulatory action. That’s why ethical digital practices are more than a best practice—they’re a competitive advantage.
Innovation, on the other hand, offers incredible opportunities. AI, automation, and predictive analytics can improve efficiency and impact. However, using them in regulated environments requires caution. Marketers must understand not only how to use these tools, but also how to keep them compliant, unbiased, and transparent. The future belongs to those who combine innovation with integrity.
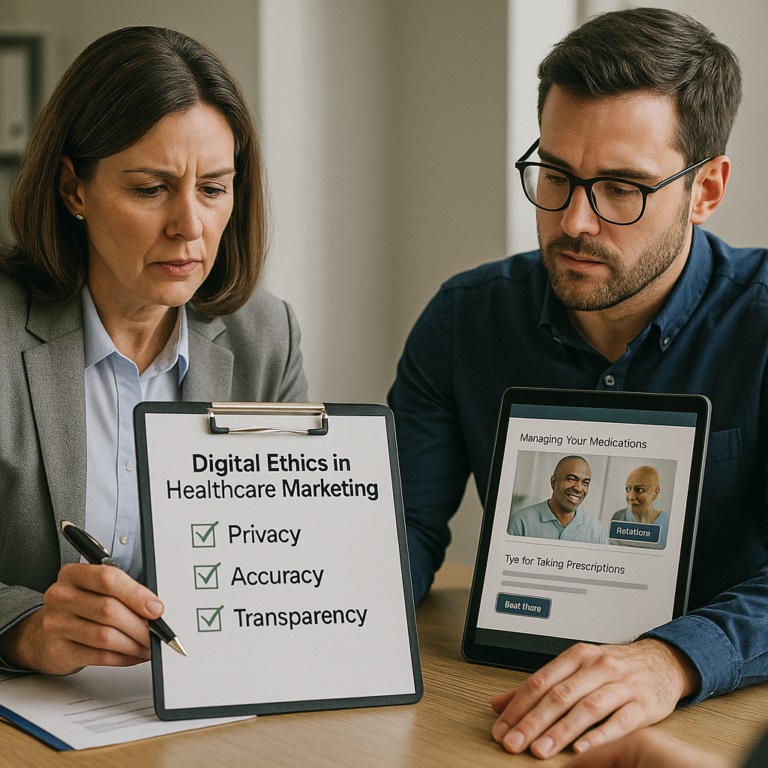
Digital Ethics in Healthcare Marketing: Doing the Right Thing
Digital ethics ensures your marketing respects privacy, avoids harm, and builds long-term trust.
- Transparent Messaging: Always share risks, limitations, and sources in consumer-friendly language.
- Privacy by Design: Collect and use data only with clear consent and purpose.
- No Clickbait: Avoid sensational headlines or misleading graphics, especially in patient content.
- Equity in Access: Ensure digital campaigns include underserved or diverse patient populations.
- Disclose Sponsorship: Clearly identify sponsored content across social media and content hubs.
Ethical marketing is not just legal—it’s essential for brand credibility and public trust.
Innovation With AI and Automation: Smarter, Faster, Safer
AI and automation bring efficiency and scalability—but only when aligned with compliance and quality.
- AI Copy Assistants: Use tools to draft content, then run it through legal and medical review.
- Predictive Targeting: Analyze behavior to predict HCP or patient needs, without invading privacy.
- Smart Scheduling: Let AI optimize send times and channels for maximum engagement.
- Regulatory Checkpoints: Embed compliance rules into automation flows to catch risky language early.
- Audit-Ready Records: Log every automated message, change, and approval for inspection-readiness.
Innovation should make your work better—not riskier. Use it to improve outcomes without cutting ethical corners.

Best Practices for Digital Marketing in Pharma & MedTech
Follow these best practices to improve your outcomes:
Build Cross-Functional Teams
Collaborate with regulatory, legal, and medical affairs from the start of each campaign.
Test and Iterate
Run small A/B tests before launching full campaigns to reduce risks and increase ROI.
Use Clear, Patient-Friendly Language
Simplify scientific terms so patients understand their options clearly.
Track KPIs That Matter
Focus on metrics like click-through rate (CTR), time-on-page, and qualified leads—not just impressions.
Localize Content
Translate and adapt campaigns for regional markets while following local regulations.
Ensure Accessibility
Design your content so users with disabilities can access it—use alt text, captions, and clear fonts.
Educate Before You Promote
Offer valuable, non-promotional content like eBooks, videos, or interactive tools.
Align with HCP Needs
Focus on solving their problems, not just selling products.
Keep Audit Trails for Every Campaign
Document every asset review, approval, and change to stay inspection-ready.
Continuously Upskill Your Team
Encourage marketers to take certified courses to stay updated on regulations and tools.
Learn Marketing in Pharma & MedTech with Pharmuni
Whether you’re a marketer, regulatory affairs professional, or product manager, digital strategy is now part of your role. But working in a highly regulated environment means you need specialized skills—Pharmuni teaches exactly that.
What You’ll Learn:
- How to create compliant campaigns for pharmaceutical and medical device products
- Key regulations: FDA, EMA, ISO 13485, MDR
- Cross-functional collaboration techniques for marketing, medical, and regulatory teams
- Real-world case studies of compliant and non-compliant campaigns
- Hands-on assignments for SEO, product launches, and pharmacovigilance messaging
With flexible online access, industry-recognized certificates, and expert-led modules, you’ll be ready to lead digital campaigns that meet regulatory and user expectations.
Pharmuni’s Marketing in Pharma & MedTech Course Prepares You for the Real World
Conclusion
Digital marketing in pharma and medtech has evolved from a “nice-to-have” into a mission-critical business function. Companies now need strategies that go beyond flashy visuals—they must also ensure ethical messaging, compliance, and personalization. As patients and healthcare professionals spend more time online, digital touchpoints have become the foundation of communication and trust.
Trends like omnichannel marketing, AI-driven personalization, and SEO-first content will continue to shape the industry. Marketers who stay ahead, embrace innovation, and follow regulations will outperform competitors and build lasting brand loyalty.
To gain a head start, upskill your team with structured, industry-specific training. Pharmuni’s course in Marketing in Pharma & MedTech is the smart choice for professionals who want to master compliant marketing and lead their brand into the future.
References:

Stephanie Männicke
Digital Marketing Especialist at Zamann Pharma Support, brings 8 years of experience in Corporate and Digital Communication. Specializing in Digital Marketing and Content Creation, Stephanie is currently focused on creating strategic content for Pharmuni's networks, especially content on topics such as recruitment, onboarding and employer branding. Outside of work, Stephanie is a mum, a crocheter and a movie fan. An avid reader and in search of expanding her knowledge, Stephanie is always looking for ways to innovate communication in the digital environment and connect people in a genuine way.

Master GxP Validation in 2026: Meaning, Key Steps, and Validated State Control
Auditors want evidence you can trace, not opinions you can explain. GxP validation links intended use, requirements, risk, and test results into one story. When

Master GMP Compliance in 2026: Meaning, Core Elements, and How to Implement
GMP compliance keeps medicines safe, consistent, and traceable across every batch. This guide explains core GMP elements, practical rollout steps, and common pitfalls. It also

History of Pharmacovigilance: From the Thalidomide Crisis (1961–2026) to GMP Oversight
Thalidomide in 1961 changed drug safety forever. Since then, pharmacovigilance has grown from crisis response to proactive risk management. Today, teams track signals, tighten reporting